ABRomics is an online community-driven platform to scale up and improve surveillance and research on antibiotic resistance from a One Health perspective.
ABRomics is an online community-driven platform to scale up and improve surveillance and research on antibiotic resistance from a One Health perspective.
Antimicrobials (also called antibiotics) are molecules capable of killing or inhibiting the growth of bacteria, fungi or parasites, leading to the treatment of infections caused by these microbes. They are essential medicine and have saved thousands of lives since they have been used. Nonetheless, bacteria, fungi or parasites have developed the capacity to resist drugs they were initially susceptible to: this is what is referred to as antimicrobial resistance (AMR). The main consequence is that infections become more difficult to treat as the number of effective antimicrobials decrease. In addition, few new antimicrobials have been released over the last two decades, creating a situation where bugs are increasingly resistant to existing drugs while the antimicrobial pipeline is drying out. We now have to improve our knowledge about how AMR emerges and spread in order to better cope with it.

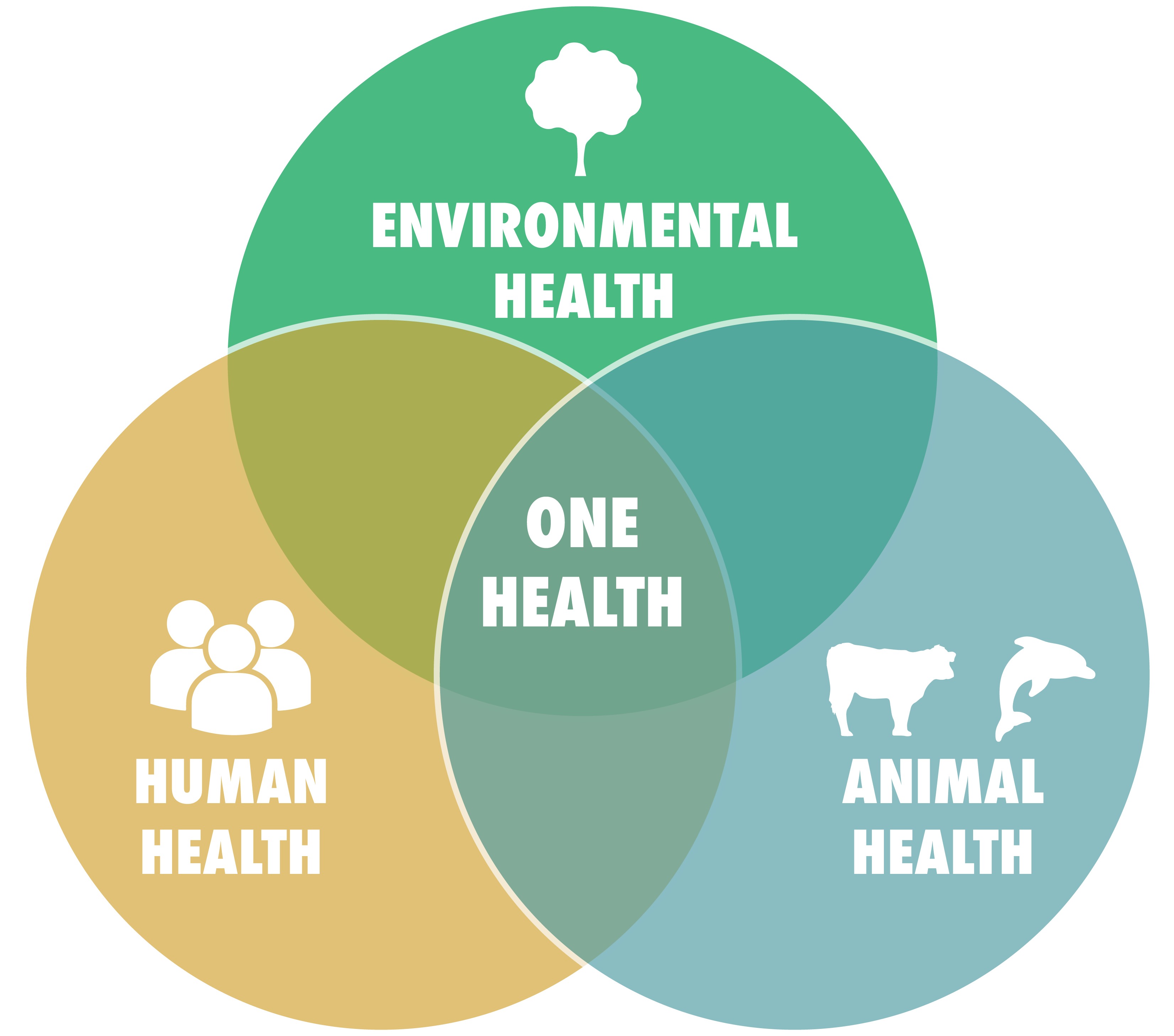
AMR emerges from the genetic changes in the genome of microorganisms (e.g. mutations) as well as genetic exchanges between. Such events are promoted by the overuse of antibiotics in Humans, but also in agriculture. Antimicrobial resistant organisms are found everywhere: in people, animals, food, plants and the environment (in water, soil and air). They can spread from person to person or between people and animals, including from food of animal origin. Poor sanitation is a strong promoter for the circulation of multidrug-resistant microorganisms between the human, animal and environmental sectors. Hence, understanding the AMR dynamics requires a global, “One Health” approach.
AMR is now a major threat to health. Recent evidence showed that AMR was responsible for more than 1 million deaths per year worldwide. As such, AMR kills more people than HIV, tuberculosis or malaria and should be considered as a top priority for research. Of note, excessive deaths attributed to AMR mainly occur in low and middle income settings. Still, multidrug-resistant microorganisms travel and also affect high-income settings. Hence, tackling AMR is a worldwide effort.
Web site World Health Organisation (WHO): https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
Web site Centers for Disease Control abd Prevention (CDC): https://www.cdc.gov/drugresistance/about.html
Article Le Grand Continent “10 points sur l’antibiorésistance”: https://legrandcontinent.eu/fr/2023/04/26/10-points-sur-lantibioresistance/
Etienne Ruppé book “Les antibiotiques c’est la panique !”: https://www.google.fr/books/edition/Les_antibiotiques_c_est_la_panique/aMiDDwAAQBAJ?hl=fr&gbpv=1&printsec=frontcover